Solutions for Hospitals
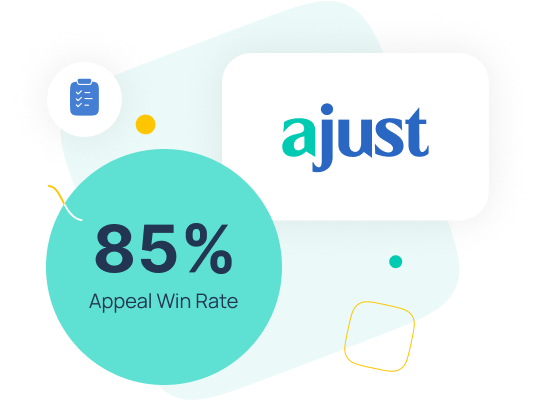
Losing money on denied medical claims should not be considered a part of doing business. With aJust’s track record of winning 85% of denied medical claims, it no longer is.

We get more claims paid
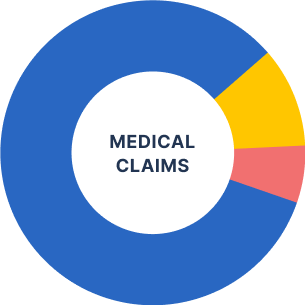
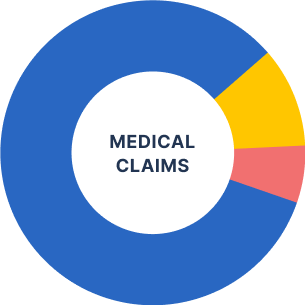
About 30 of every 100 medical claims are rejected by insurers. On average, about 13 of those are corrected and reprocessed and paid by the insurer. However, 17 claims are never paid by the insurer and become the responsibility of the patient to pay often resulting in the debt being written off or being sent to debt collection.
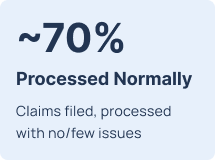
~70%
Processed Normally
Claims filed, processed with no/few issues

~70%
Processed Normally
Claims filed, processed with no/few issues
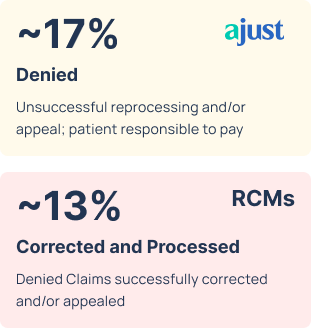
~17%
Denied/Patient Responsibility
Unsuccessful reprocessing and/or appeal; patient responsible to pay
~13%
Corrected and Processed
Denied Claims successfully corrected and/or appealed
Why aJust
Approximately 1 in 6 healthcare claims in the U.S. (around 500 million claims) are denied annually. And 2 of 3 claims are never successfully re-processed/appealed because of resource constraints and process complexity. As a result, physicians and clinics suffer financially as payment is significantly delayed or never made at all.
Let aJust fight for you! With an 85% success rate, aJust ensures rightful payment for denied medical claims. And aJust works on performance – we get paid only when you are.
aJust pays 4x more than debt collection
Referring a patient with a denied medical claim to debt collection has always been the last and only option for many physicians/clinics. But aJust now provides another alternative – and with much better results for you and your patients.
Appealing a denied claim keeps your Patient out of debt and maintains a positive relationship with them.
| Debt collection |
 |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Paid commission on success only |
Yes |
Yes |
|||||||||||||||||||||
|
Fee (%) of the recovered amount |
25% - 40% |
20% |
|||||||||||||||||||||
|
Time to Resolution |
4 - 12 months |
2 - 3 months |
|||||||||||||||||||||
|
Success rate in recovering funds |
25% |
85% |
|||||||||||||||||||||
|
Average recovery on $100 of value |
$15 |
$68 |
aJust only charges for appeals we win
aJust’s fee is based on the actual amount that we recover from the insurance provider. There is no fee if aJust is unsuccessful in getting a denied claim approved.


Sit back and relax
Instead of having your team go through the agony of dealing with health insurers regarding denied claims, aJust’s seasoned team will handle the entire process for you.
Our team are experts in winning appeals
aJust has a team of professionals dedicated solely to appealing denied healthcare claims. They know how to navigate the incredibly confusing health insurance environment, and win.


We win, a lot!
Almost 2 of 3 denied claims are never successfully re-processed/appealed because of resource constraints and process complexity. As a result, hospitals suffer financially as payment is significantly delayed or never made at all. Don’t let leave money on the table and boost your profit with aJust!
Let aJust help you and your Patients solve this financial nightmare
We help people every single day with their medical claims, let us help your practice too.
The Trust We Earned
“I had won my appeal. Blue Shield would now have to pay the bill. What a relief. I would still be making payments to the collection agency if I had not found ajust Solutions. Don't hesitate, let ajust Solutions do the fighting for you when you are up against "Big Medical".”
“aJust Solutions reduced my bill by 75%. They were extremely kind and helpful. They certainly earned their money. I would recommend them to anyone.”
“NO, I did not have to pay the provider anything. The price of working with aJust Solutions is completely worth it. If you have issues with claims being denied by your insurance, I would highly recommend contacting aJust Solutions and let them assist you.”
Track record of success
4.8/5
Rating on Google Reviews
85%
We win of denied claims we appeal
Decades
of experience within the team
Expertise
Filling and winning Appeals and Independent Medical Reviews
All Major Insurers
All 50 States
aJust provides everything needed
to get started
0
Electronic brochure introducing
aJust services

0
Intro email of aJust
to patients

OPTIONAL
Co-branded aJust/Clinic landing page on aJust website for your patients
Track record
of success

4.8/5
Rating on Google Reviews
85%
We win of denied claims we appeal
Expertise
Filling and winning Appeals and Independent Medical Reviews
All Major Insurers
All 50 States
Decades
of experience within the team
What our clients are saying
“I tried appealing my claim over and over. I even had an advocate at the insurance company that was supposed to be helping me and they just kept denying it. Frankly, I was about to give up. And I found aJust Solutions on the internet and I made a phone call and we started from there. aJust Solutions did everything. They simply asked me for the information that they needed and I sent it to them and they did all the work.”
Leo S.
aJust Customer
Contact Us
We are experts in navigating the complicated process of getting
denied healthcare claims paid. Let us help.
